How to Achieve Hormonal Balance Naturally
Your endocrine system orchestrates over 50 distinct hormones daily, each serving as a precise chemical messengers that regulate essential physiological processes throughout your body. At DrStileRx, our clinical expertise centers on understanding how these bioactive compounds influence circadian rhythms, metabolic function, neurotransmitter activity, and cellular communication pathways.
Endocrine disruption presents through multiple symptom clusters. Clinical data indicate that perimenopausal and menopausal women report an average of 11 distinct symptoms, though fewer than 50% receive adequate preparation for managing these transitions. The gut-hormone axis proves equally significant, where over 100 trillion microbial organisms generate metabolites that either support or compromise endocrine function. Weight regulation often reflects underlying hormonal dysregulation, particularly affecting insulin sensitivity and reproductive hormone cascades.
Dr. Stile and our clinical team at DrStileRx.com provide evidence-based hormone-optimization protocols and therapeutic interventions to restore endocrine balance. Our approach addresses hormone imbalance presentations in both male and female patients, examines the nutritional influences on hormone synthesis, and evaluates candidacy for appropriate hormone replacement therapy. Persistent fatigue, mood instability, or unexplained weight fluctuations often signal endocrine dysfunction—accurate assessment of your hormone profile establishes the foundation for targeted therapeutic intervention and sustained wellness outcomes.
What are hormones, and how do they affect your health?
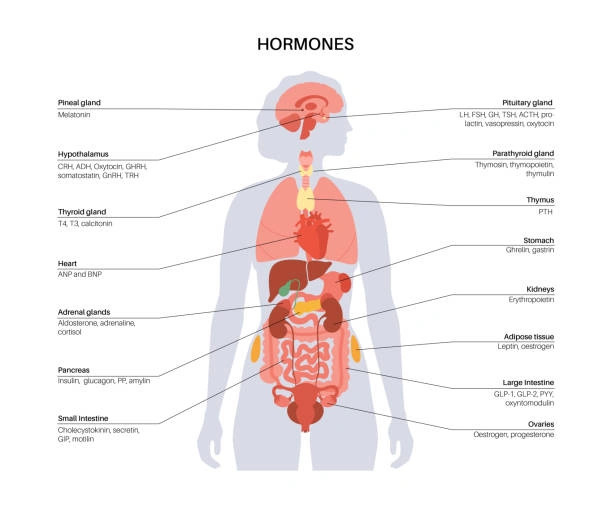
The endocrine system operates through sophisticated biochemical signaling, in which hormones function as molecular messengers that orchestrate cellular activity throughout your body. DrStileRx specializes in hormone optimization because we recognize that endocrine balance serves as the cornerstone of optimal health. Current scientific research has documented over 50 hormones within human physiology, each contributing specific regulatory functions essential for vitality and wellness.
Understanding the role of chemical messengers
These bioactive compounds circulate through your bloodstream, delivering precise instructions to target tissues and organs. Our clinical approach at DrStileRx.com emphasizes patient education regarding how these potent molecules modulate critical physiological processes—growth patterns, metabolic rate, sexual function, reproductive cycles, and neurochemical balance.
Hormonal activity requires remarkably small concentrations to generate substantial physiological responses throughout cellular systems. Each hormone molecule operates through receptor-specific binding mechanisms, functioning like molecular keys designed for particular cellular locks. This binding event initiates intracellular signaling cascades that modify existing protein function or activate gene expression for new protein synthesis.
Dr. Stile explains, “Hormonal optimization creates the foundation for sustained wellness. When your endocrine system functions efficiently, metabolic processes remain stable, emotional regulation improves, muscular strength is maintained, and sleep quality becomes restorative”.
Why hormone levels fluctuate naturally
Endocrine function exhibits natural variability across different life stages. Dr. Stile identifies several periods associated with significant hormonal transitions:
- Pubertal development
- Pregnancy and postpartum periods
- Menopausal transition
Cyclical patterns also influence hormone concentrations at daily and monthly time scales. Women experience predictable hormonal shifts throughout menstrual cycles. The follicular phase shows rising estrogen levels until ovulation, followed by a decline in estrogen while progesterone levels increase.
Age-related changes significantly impact endocrine function. Testosterone production begins a gradual decline in men during their mid-twenties, with one in three men over 45 showing low testosterone levels on laboratory assessment. Women experience accelerated estrogen reduction between the ages of 45 and 55 during the menopausal transition.
Additional factors influencing hormonal stability include:
- Chronic stress exposure
- Pharmaceutical interventions
- Environmental chemical exposure
Common hormones involved in daily functions
Our DrStileRx hormone optimization program focuses on key endocrine factors that directly impact daily wellness:
Estrogen: The primary female sex hormone regulating ovulatory cycles, menstrual function, mammary tissue development, and bone mineral density. Men also produce smaller quantities for various physiological functions.
Testosterone: Essential for libido maintenance, body composition, muscular strength, skeletal health, and erythropoiesis in both sexes.
Insulin: A Pancreatic hormone facilitating glucose uptake for cellular energy production and maintaining glycemic control. Impaired insulin function or resistance can progress to metabolic dysfunction or diabetes.
Cortisol: Known as the stress hormone, cortisol regulates metabolic processes, blood pressure, inflammatory responses, and memory formation. Dr. Stile notes that chronic cortisol elevation contributes to anxiety disorders, sleep disruption, and autoimmune conditions.
Thyroid hormones: These regulate basal metabolic rate, growth patterns, developmental processes, and thermoregulation. Our hormone therapy clinic recognizes thyroid dysfunction as a primary factor in weight management challenges and energy deficits.
Growth hormone: Secreted by the pituitary gland, this hormone stimulates cellular growth and regeneration during development while supporting metabolic function throughout adulthood.
Dr. Stile emphasizes that “endocrine stability requires careful clinical management, which is why specialized hormone therapy provides optimal outcomes”. DrStileRx develops individualized treatment protocols through detailed laboratory assessment and comprehensive evaluation before implementing targeted therapeutic interventions for sustained hormonal wellness.
What are the signs of a hormone imbalance in men and women?
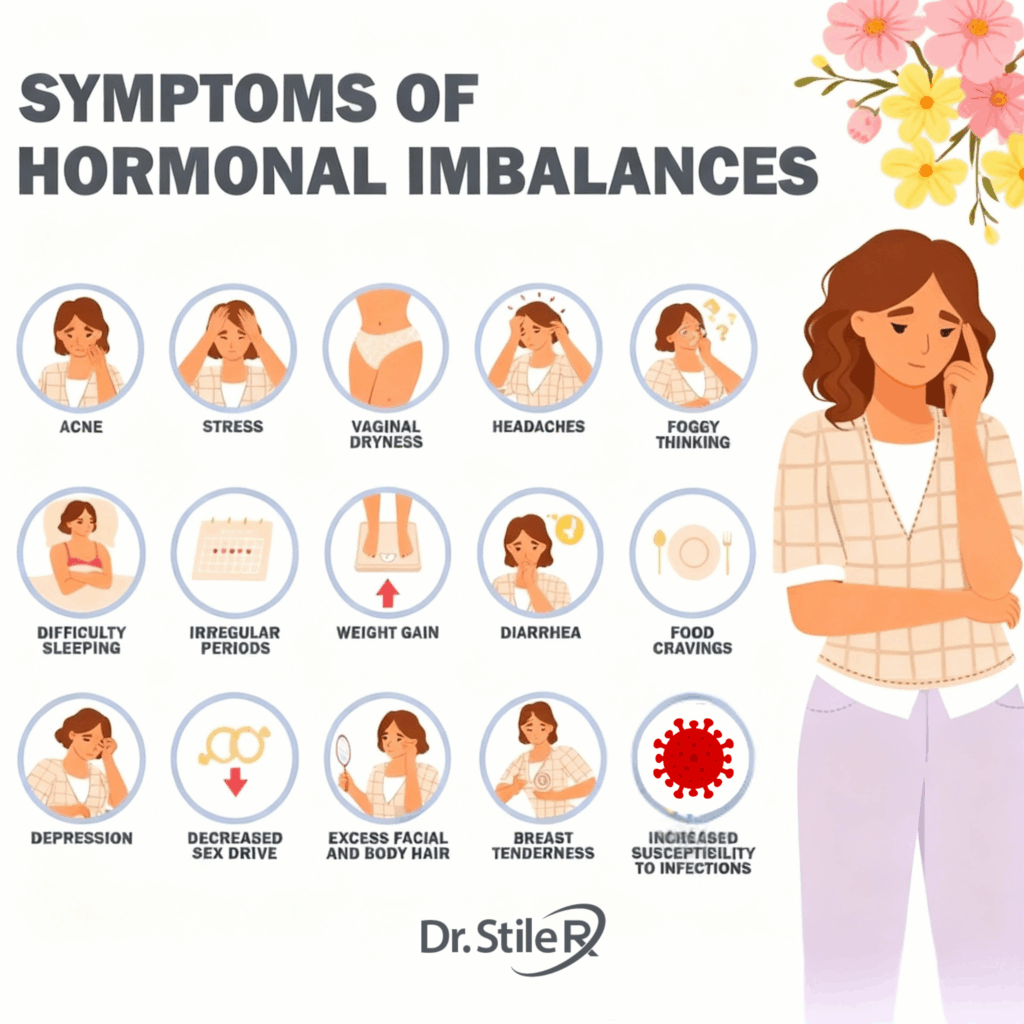
Early identification of endocrine dysfunction enables prompt intervention and prevents progressive health deterioration. Dr. Stile at DrStileRx recognizes that hormonal messengers influence multiple physiological systems simultaneously. Given the complexity of over 50 different hormones operating within your body, imbalances present through diverse symptom patterns.
Mood swings and fatigue
Chronic exhaustion frequently represents the initial manifestation of hormonal dysregulation. At DrStileRx.com, our clinical practice regularly encounters patients experiencing profound fatigue secondary to endocrine imbalances. Sustained stress response activation disrupts cortisol rhythms, leading to simultaneous energy depletion and hyperarousal.
“Patients frequently describe a paradoxical ‘tired but wired’ sensation when experiencing hormone disruption,” observes Dr. Stile. “Physical exhaustion coexists with an inability to achieve restorative rest.”
Endocrine fluctuations commonly trigger psychological symptoms, including:
- Unexplained anxiety or depressive episodes
- Emotional lability and irritability
- Cognitive impairment or mental clarity issues
- Persistent hopelessness
Female patients often experience symptom intensification during luteal phases or perimenopausal transitions as progesterone and estrogen levels fluctuate significantly. Male patients with testosterone deficiency typically report mood depression and heightened anxiety responses.
Weight gain or loss
Unexplained changes in body weight frequently indicate underlying hormonal pathology. Dr. Stile notes, “When patients report weight gain despite unchanged dietary and activity patterns, endocrine assessment becomes imperative.”
Multiple hormone-related conditions affect metabolic regulation:
- Hypothyroidism: Reduces metabolic rate, promoting weight accumulation
- Cushing’s syndrome: Causes rapid weight distribution changes, particularly in the facial, abdominal, and cervical regions
- Menopause: Hormonal transitions decrease metabolic efficiency, increasing susceptibility to weight gain susceptibility
Minor hormonal shifts can produce significant metabolic consequences. Insulin resistance—cellular insensitivity to insulin signaling—contributes to weight gain and may progress to diabetes mellitus.
DrStileRx’s hormone optimization program addresses these metabolic challenges systematically. Perimenopausal women aged 35-45 experience particular vulnerability, with declining progesterone triggering anxiety, sleep dysfunction, and weight fluctuations.
Sleep disturbances and libido changes
Sleep-hormone relationships operate bidirectionally—endocrine imbalances disrupt sleep architecture while sleep deprivation exacerbates hormonal dysfunction. Female patients demonstrate greater susceptibility to this connection, with insomnia prevalence significantly exceeding male rates.
Progesterone functions as a neurosteroid with sedative properties. Declining levels during perimenopause or premenstrual periods consistently impair sleep quality. Concurrently, estrogen fluctuations trigger vasomotor symptoms like night sweats and hot flashes, causing frequent sleep interruptions.
Reduced libido affects approximately 20% of men and higher percentages of women throughout their lifespans. Primary hormone-related etiologies include:
- Testosterone deficiency in men results in diminished sexual interest and erectile dysfunction
- Estrogen decline in women causes vaginal atrophy and sexual discomfort
- Thyroid dysfunction affects both energy levels and sexual desire across genders
“Sexual dysfunction requires clinical evaluation rather than dismissal as age-related decline,” Dr. Stile emphasizes. “DrStileRx patients learn that decreased libido often reflects correctable endocrine imbalances.”
Skin issues and hair thinning
Integumentary and follicular changes provide visible markers of hormonal status. Hormonal acne typically affects the cheeks, jawline, and chin, particularly among women experiencing fluctuations in estrogen and progesterone.
Elevated cortisol levels exacerbate inflammatory dermatological conditions, such as eczema, by suppressing the immune system and increasing inflammatory mediators. Melasma—hyperpigmented facial patches—frequently results from hormonal changes during pregnancy or oral contraceptive use.
Hair alterations often cause significant patient distress. Hyperthyroidism affects up to 50% of patients with diffuse alopecia, while hypothyroidism causes hair loss in 33% of cases. Menopausal women experience androgenetic alopecia as the protective estrogen effects diminish.
Men with hypogonadism commonly develop reduced body hair density and scalp thinning, while women with polycystic ovary syndrome may develop hirsutism due to elevated androgen levels.
Dr. Stile advises DrStileRx patients that these visible manifestations typically respond favorably to hormone optimization therapy once underlying imbalances are properly identified and targeted through individualized protocols.
What causes a hormonal imbalance, and when should you be concerned?
Identifying the root causes of endocrine dysfunction requires clinical expertise and systematic evaluation, as Dr. Stile at DrStileRx emphasizes in hormone optimization practice. While hormonal fluctuations occur naturally throughout life, specific triggers can create persistent imbalances requiring professional intervention.
Lifestyle and environmental triggers
Our clinical experience at DrStileRx.com demonstrates that daily habits profoundly influence endocrine function. Chronic stress emerges as a primary disruptor, elevating cortisol production and, when sustained over time, subsequently interfering with thyroid hormones, estrogen, and progesterone.
“Clinical assessment reveals that patients often underestimate how environmental toxins impact their hormone health,” explains Dr. Stile. “These endocrine-disrupting chemicals (EDCs) present significant challenges through everyday exposures.”
Common sources of endocrine disruption include:
- BPA-containing plastics and containers
- Agricultural pesticides and industrial compounds
- Phthalates in personal care formulations
- Synthetic fragrances in household products
Exercise patterns and dietary choices create additional pathways to hormonal disruption. Both excessive training protocols and sedentary behavior can compromise reproductive hormone synthesis. Sleep architecture is equally critical, as disrupted rest patterns create a cascade in which hormone imbalances impair sleep quality, further compromising endocrine function.
Pharmaceutical interventions, particularly oral contraceptives and corticosteroid therapies, may induce temporary hormonal modifications. Our hormone optimization program incorporates a thorough lifestyle assessment before developing individualized therapeutic protocols.
Medical conditions like PCOS or thyroid disorders
Polycystic Ovary Syndrome (PCOS) represents a common endocrine disorder characterized by irregular menstrual cycles, elevated androgen levels, and metabolic dysfunction. Insulin resistance occurs in 50-80% of women with PCOS, establishing a complex interplay where hormonal imbalances exacerbate metabolic complications.
Thyroid pathologies constitute another frequent source of endocrine disruption. Hypothyroidism manifests when thyroid hormone production becomes insufficient, while hyperthyroidism results from excessive thyroid hormone synthesis. Both conditions produce widespread physiological effects due to thyroid hormones’ regulatory influence across multiple organ systems.
Autoimmune disorders frequently target hormone-producing tissues. “Our clinical practice regularly identifies autoimmune conditions such as Hashimoto’s thyroiditis or Graves’ disease underlying persistent hormonal symptoms,” notes Dr. Stile. “These disorders prompt immune system attacks against endocrine glands, compromising normal hormone synthesis”.
Aging and perimenopause
Age-related endocrine changes affect all individuals, primarily through progressive decline in sex hormone production. Women experience perimenopause, the transitional period preceding menopause, when estrogen and progesterone levels fluctuate unpredictably. This transition typically spans four years, from the mid-30s to the mid-50s, though it can extend to eight years.
Perimenopausal manifestations include menstrual irregularities, hot flashes affecting 35-50% of women, and sleep disruption reported by approximately 40% of patients. Notably, 10-20% develop mood-related symptoms during this transition.
Male patients experience a gradual testosterone decline at approximately 1% annually beginning in their 30s. By age 80, 40-50% of men demonstrate testosterone levels below normal ranges for healthy young adults.
Several factors may accelerate perimenopausal onset:
- Tobacco use (advances menopause 1-2 years)
- Genetic predisposition to early menopause
- Oncological treatments
- Surgical interventions, including hysterectomy or oophorectomy
- Thyroid dysfunction and autoimmune conditions
Professional consultation at DrStileRx becomes warranted when symptoms compromise quality of life, persist despite lifestyle modifications, or co-occur with additional health concerns. Our diagnostic hormone testing identifies specific imbalances, enabling the development of personalized therapeutic protocols aligned with your individual health profile.
How can diet help balance your hormones naturally?
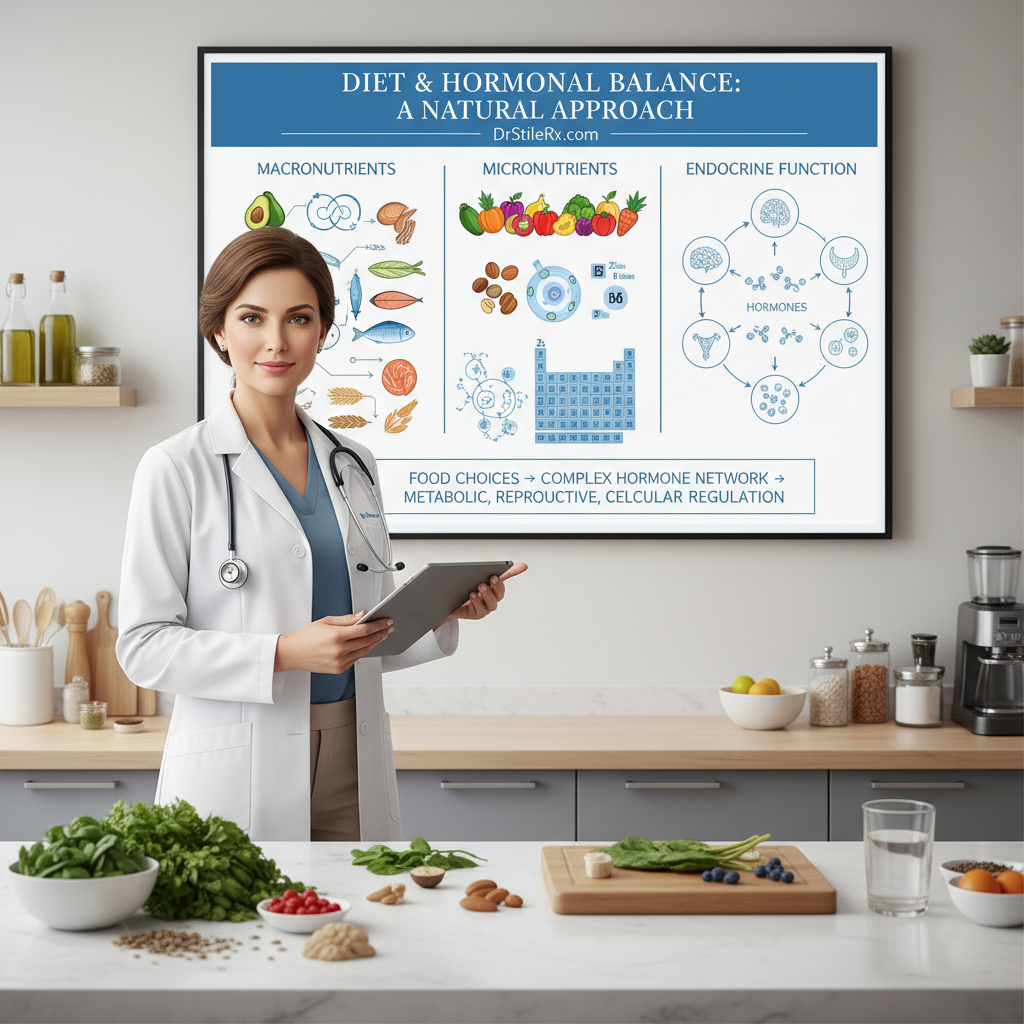
Nutritional interventions represent a foundational approach to hormone regulation, as Dr. Stile demonstrates at DrStileRx. The biochemical relationships among macronutrients, micronutrients, and endocrine function create opportunities for therapeutic dietary modifications. Each food choice influences the complex network of over 50 hormones governing metabolic processes, reproductive function, and cellular signaling pathways.
Best foods for hormone health
“Our clinical approach at DrStileRx.com prioritizes nutrient-dense whole foods that provide the raw materials necessary for optimal hormone synthesis,” explains Dr. Stile. Mediterranean dietary patterns demonstrate significant therapeutic potential for hormone regulation. Research documenting women following this nutritional protocol experienced a 40% decrease in total estrogen levels compared to controls maintaining standard dietary patterns.
Dietary fiber functions as a critical regulator of hormone metabolism through multiple mechanisms:
- Enhancing hepatic estrogen conjugation and fecal elimination
- Modulating gut microbiome composition and metabolic activity
- Reducing enterohepatic recirculation of steroid hormones
Complete protein sources provide essential amino acid profiles required for peptide hormone synthesis. Dr. Stile emphasizes that high-quality proteins from eggs, wild-caught fish, organic poultry, and fermented soy provide all nine essential amino acids while supporting satiety by regulating ghrelin.
Essential fatty acids serve as precursors for steroid hormone biosynthesis, particularly supporting reproductive and stress hormone pathways. Monounsaturated fats from avocados and olive oil, along with omega-3 fatty acids from cold-water fish, facilitate hormone production while promoting metabolic efficiency.
Can diet affect estrogen and testosterone?
Dietary composition demonstrates measurable effects on circulating sex hormone concentrations. Western dietary patterns characterized by processed meats, refined carbohydrates, and industrial seed oils correlate with elevated estrogen levels across multiple population studies. Plant-forward nutritional approaches consistently produce lower estrogen concentrations and reduced risk profiles for hormone-dependent malignancies.
Phytoestrogens represent bioactive plant compounds with selective estrogen receptor modulator properties. These naturally occurring molecules from legumes, flaxseeds, and cruciferous vegetables demonstrate dual regulatory effects—providing mild estrogenic activity when endogenous levels are low while competing for receptor binding when estrogen concentrations are elevated. Dr. Stile notes that phytoestrogens at DrStileRx function as natural hormone modulators rather than simple hormone mimics.
Male patients often express concerns regarding soy consumption and testosterone levels. A meta-analysis of 32 controlled trials reveals no significant effect on circulating or bioavailable testosterone in healthy men consuming moderate amounts of isoflavones. However, one long-term study documented decreased free testosterone in men consuming 141 mg of isoflavones daily over 12 months.
Foods to avoid for hormone optimization
“Our hormone therapy protocols at DrStileRx include specific dietary restrictions targeting foods known to disrupt endocrine signaling,” states Dr. Stile. Trans fatty acids from partially hydrogenated oils promote insulin resistance and systemic inflammation, creating metabolic conditions that interfere with hormone receptor sensitivity.
Alcohol consumption requires careful consideration due to its effects on cortisol regulation and adipose tissue distribution, particularly promoting visceral fat accumulation. Additionally, alcohol consumption can elevate estradiol concentrations in women, with effects most pronounced during the ovulatory phase.
Processed food products containing preservatives, artificial additives, and packaging-derived chemicals, such as phthalates, pose ongoing endocrine-disrupting risks. Dr. Stile’s nutritional recommendations include:
- Eliminating refined sugars that trigger insulin dysregulation
- Choosing organic dairy products to avoid synthetic hormone residues
- Moderating red meat intake, which correlates with increased estrogen metabolism
Before implementing significant dietary modifications, Dr. Stile recommends comprehensive hormone testing at DrStileRx to establish baseline measurements and identify specific nutritional targets for your individual hormone optimization program.
How do sleep and stress impact hormone levels?
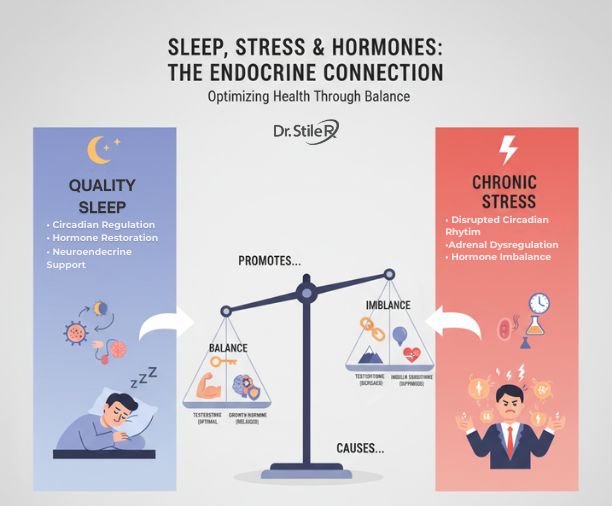
Sleep architecture and stress physiology maintain intricate relationships with endocrine function, a critical consideration Dr. Stile addresses in our hormone optimization protocols at DrStileRx. Quality sleep hygiene and stress modulation are fundamental pillars of effective hormone-restoration programs. Your neuroendocrine system requires optimal circadian regulation and calibrated stress responses to maintain physiological homeostasis.
The sleep-hormone connection
Sleep serves as an active regulatory process for hormone synthesis rather than a passive state of rest. Dr. Stile at DrStileRx.com explains, “Restorative sleep enables your cortisol reaches its peak within 30 minutes of waking, initiating the cascade of thyroid and reproductive hormone activation”.
Circadian biology governs hormone release patterns across 24-hour cycles. Nocturnal sleep phases facilitate the production and regulation of multiple hormones controlling growth factors, tissue repair, appetite modulation, and stress response mechanisms. Sleep fragmentation disrupts these precisely timed endocrine processes.
Sleep deprivation particularly affects:
- Growth hormone – Secreted predominantly during slow-wave sleep stages for anabolic tissue processes
- Cortisol – Requires nocturnal suppression for proper recovery, but remains elevated with sleep dysfunction
- Appetite-regulating hormones – Sleep restriction dysregulates leptin and ghrelin, promoting increased caloric intake
- Sex hormones – Sleep disorders create imbalances in estrogen and testosterone production
Single episodes of sleep restriction can compromise insulin sensitivity, potentially contributing to metabolic dysfunction and weight accumulation.
Cortisol and adrenal fatigue
The adrenal cortex produces multiple steroid hormones, with cortisol serving as the primary glucocorticoid. Normal cortisol secretion follows a diurnal pattern featuring morning peak levels for arousal and evening nadir for sleep preparation. Disruption of this rhythm creates widespread physiological consequences.
“Adrenal fatigue” has become a commonly referenced condition suggesting chronic stress depletes adrenal function, resulting in hypocortisolism and associated symptoms including cognitive impairment, fatigue, and mineral cravings. Dr. Stile notes that current scientific literature lacks substantive evidence supporting this diagnostic framework—systematic reviews of 58 studies found no validated connection between adrenal insufficiency and fatigue symptomatology.
Clinical research confirms that salivary cortisol measurements showed no significant differences between fatigued and healthy populations in 61.5% of investigations. Cortisol replacement therapy for unsubstantiated adrenal fatigue carries serious risks, including bone demineralization, glucose intolerance, and cardiovascular complications.
Does stress cause hormone imbalance?
Chronic stress exposure directly compromises endocrine equilibrium. Dr. Stile observes that persistent stress activation frequently underlies hormonal dysregulation in our patient population. “Modern lifestyle demands create continuous physiological strain. The majority of patients presenting with hormone imbalances demonstrate elevated cortisol as the primary disruptor, subsequently affecting downstream endocrine pathways,” explains Dr. Stile.
Stress activation triggers the hypothalamic-pituitary-adrenal (HPA) axis, amplifying multiple hormone production pathways. Stress hormones can rise two- to fivefold during acute stress responses. This system should activate transiently, but chronic stress maintains persistent activation.
Prolonged stress compromises multiple endocrine systems:
- Reproductive axis – Stress suppresses gonadotropin-releasing hormone and sex steroid production, disrupting menstrual function and fertility
- Thyroid regulation – Stress typically reduces thyroid hormone conversion with decreased T3 and T4 concentrations
- Growth hormone secretion – Acute physical stress increases GH dramatically, while chronic psychological stress often produces GH insufficiency
- Glucose metabolism – Stress may reduce insulin effectiveness while increasing counter-regulatory hormones, promoting hyperglycemia.
Persistent activation of the stress response and chronic cortisol exposure can compromise virtually all physiological systems. This increases risk for anxiety disorders, depressive episodes, gastrointestinal dysfunction, sleep disorders, weight gain, and cardiovascular disease.
Our DrStileRx hormone optimization program identifies and addresses stress-related endocrine disruption through comprehensive diagnostic evaluation and individualized therapeutic protocols designed to restore hormonal equilibrium.
What role does exercise play in hormone regulation?
Physical activity functions as a potent therapeutic modality for hormone regulation, as Dr. Stile explains through our clinical protocols at DrStileRx.com. Exercise physiology research demonstrates that targeted movement strategies generate specific endocrine responses that optimize hormonal cascades throughout your body’s regulatory systems.
Types of workouts that support hormone health
“Daily physical activity volume and intensity patterns directly influence endocrine system responses,” Dr. Stile notes from our hormone optimization program outcomes. Exercise modalities produce distinct hormonal effects, requiring strategic programming for optimal results:
Resistance training protocols: Full-body strength sessions 2-3 times weekly stimulate growth hormone and testosterone production—essential anabolic hormones for muscle protein synthesis and metabolic regulation.
High-intensity interval training (HIIT): Brief 12-20 minute sessions performed three times weekly provide maximum hormone-balancing benefits without excessive physiological stress. Extended HIIT protocols can elevate cortisol unnecessarily.
Parasympathetic activation practices: Yoga and Pilates modalities engage the relaxation response, effectively reducing cortisol elevation and supporting stress hormone recovery.
Aerobic base building: Consistent walking sessions, 4-5 days weekly, establish a metabolic foundation while supporting insulin sensitivity.
How movement affects insulin and cortisol
Exercise initially triggers acute stress responses, temporarily elevating cortisol levels. This hormetic stress response proves beneficial—training your body’s stress recovery mechanisms to improve cortisol regulation. Clinical evidence shows that regular exercisers maintain lower baseline cortisol levels than sedentary populations.
Physical activity demonstrates remarkable efficacy in optimizing insulin. Active muscle tissue increases glucose uptake, prompting insulin release to facilitate glucose transport into cells. Regular exercise enhances insulin receptor sensitivity, countering insulin resistance patterns and improving glycemic control.
Exercise prescription requires careful balance, particularly with high-intensity protocols. “HIIT programming requires adequate recovery periods between sessions—limiting frequency to 2-3 weekly sessions based on individual fitness capacity,” Dr. Stile advises in our treatment protocols.
Exercise recommendations for hormone optimization after 40
Age-related hormonal changes necessitate modified exercise programming. Our DrStileRx hormone therapy clinic protocols emphasize:
- Resistance training prioritization—critical for maintaining bone mineral density and lean muscle mass during hormonal transitions
- Weekly aerobic targets of 150 minutes moderate-intensity activity (distributed as 30-minute sessions across 5 days)
- Extended recovery intervals between high-intensity sessions—aging physiology requires longer adaptation periods
- Bioindividual programming based on current hormonal status and symptoms
“Exercise represents a physiological stressor requiring careful management within your overall hormone balance strategy,” Dr. Stile cautions. Our clinical approach includes comprehensive hormone testing before implementing exercise protocols, ensuring your movement prescription supports rather than disrupts your endocrine optimization goals.
When should you consider hormone therapy or HRT?
Hormone replacement therapy represents a clinical intervention that addresses persistent endocrine dysfunction when lifestyle modifications prove insufficient. Dr. Stile at DrStileRx specializes in evaluating patients for hormone therapy candidacy, particularly those experiencing significant quality-of-life impacts from hormonal imbalances.
What is hormone replacement therapy?
Hormone replacement therapy (HRT) involves pharmaceutical interventions designed to restore hormonal levels in postmenopausal women whose endogenous hormone production has declined. At DrStileRx.com, our clinical protocols address vasomotor symptoms such as hot flashes and urogenital atrophy through targeted hormonal supplementation. Contemporary medical practice refers to this intervention as hormone therapy (HT), particularly for patients initiating treatment after age 50.
Beyond symptom management, HRT provides therapeutic benefits, including bone density preservation and fracture risk reduction in postmenopausal populations. Treatment modalities include:
- Systemic hormone therapy – utilizing oral, transdermal, or parenteral delivery systems for whole-body hormonal support
- Local vaginal estrogen therapy – low-dose formulations targeting specific urogenital symptoms with minimal systemic absorption
Bioidentical hormone therapy vs traditional HRT
Dr. Stile’s hormone optimization protocols prioritize bioidentical hormones that are molecularly similar to endogenous estrogen and progesterone. These plant-derived preparations, such as those from soy and wild yam, contrast with synthetic hormone analogues derived from non-human sources.
This molecular congruence proves clinically significant because bioidentical formulations replicate the exact chemical structure of naturally occurring hormones. FDA-approved bioidentical preparations are available, alongside custom-compounded formulations prepared by specialized pharmacies. However, compounded preparations lack extensive long-term safety data compared to standardized pharmaceutical products.
Safe hormone therapy options for women and men
Women with intact uteri require combined estrogen-progestogen therapy to prevent endometrial hyperplasia and malignancy risk. Post-hysterectomy patients typically receive estrogen monotherapy. DrStileRx hormone specialists determine the optimal delivery method—oral, transdermal, or vaginal—based on individual symptom profiles and risk assessments.
Male patients experiencing androgen deficiency benefit from testosterone replacement protocols addressing fatigue, body composition changes, and diminished libido.
When to start hormone therapy
Clinical timing proves crucial for hormone therapy initiation. Research demonstrates favorable risk-benefit profiles when HRT commences before age 60 or within the initial decade following menopause. This therapeutic window provides protective effects against osteoporosis, cardiovascular disease, mood disorders, and cognitive decline associated with estrogen deficiency.
Premature or early menopause (onset before age 45) necessitates particular consideration for HRT, given the extended duration of estrogen deprivation compared to age-appropriate menopausal transitions. DrStileRx evaluates individual health profiles, symptom severity, and personal risk factors to determine each patient’s candidacy for hormone therapy.
How can you test and track your hormone levels?
Accurate hormone assessment establishes the foundation for effective endocrine optimization, as Dr. Stile emphasizes throughout our clinical practice. At DrStileRx’s hormone optimization program, our diagnostic approach centers on precise measurement methodologies that reveal your individual hormone profile and guide targeted therapeutic interventions.
How to check your hormone levels at home or with a doctor
Clinical hormone evaluation requires sophisticated laboratory analysis, as endocrine glands secrete hormones directly into the circulation. Dr. Stile employs multiple diagnostic modalities for thorough endocrine assessment:
- Serum analysis: Primary diagnostic method quantifying testosterone, estrogen, cortisol, and thyroid hormone concentrations
- Salivary biomarkers: Specialized testing measuring free hormone fractions, including estradiol, progesterone, and testosterone
- Urinary metabolites: Advanced testing protocols for specific endocrine evaluations
Consumer-directed testing options have expanded accessibility through capillary blood sampling and saliva collection systems. However, these approaches may lack clinical precision, as hormone concentrations exhibit significant circadian variability.
Hormone imbalance quiz and lab tests
Patient assessment at DrStileRx.com begins with detailed symptom evaluation questionnaires targeting specific endocrine dysfunctions. These clinical screening tools evaluate presentations associated with:
- Estrogen excess or deficiency states
- Androgen insufficiency
- Thyroid dysfunction
- Adrenal axis dysregulation
Laboratory diagnostics provide definitive clinical validation. Your hormone specialist conducts a thorough medical evaluation and physical examination and orders targeted endocrine panels. Hormone concentrations exhibit marked diurnal fluctuation, necessitating specialized testing protocols such as glucose tolerance assessments or insulin sensitivity evaluations.
Personalized hormone therapy plans based on results
DrStileRx develops customized therapeutic protocols based on your specific endocrine profile. Our individualized approach begins with extensive laboratory evaluation, followed by comprehensive clinical consultations that address symptomatology, medical history, and treatment objectives.
Laboratory findings indicating hormonal deficiency typically respond well to targeted hormone replacement protocols. Elevated hormone concentrations may require pharmaceutical intervention, surgical management, radiation therapy, or multimodal treatment strategies.
Conclusion
Hormone optimization represents a cornerstone of sustainable wellness and long-term health outcomes. This clinical guide demonstrates how endocrine function influences multiple physiological systems simultaneously. Dr. Stile emphasizes that hormone literacy empowers patients to make informed decisions about their health trajectory. Properly regulated hormones function as integrated networks, coordinating sleep architecture, energy metabolism, mood stability, and metabolic processes.
Hormone health operates within interconnected biological systems. Nutritional choices, stress management protocols, sleep hygiene, and physical activity patterns all influence endocrine function. Dr. Stile advocates nutrient-dense dietary approaches emphasizing fiber intake, essential fatty acids, and a complete amino acid profile to support endogenous hormone synthesis. Concurrently, evidence-based stress reduction techniques help normalize cortisol secretion patterns that otherwise cascade through other hormone pathways.
Sleep quality demands particular clinical attention. Restorative sleep cycles enable precise hormone regulation during specific nocturnal phases. This relationship explains why sleep disruption frequently precipitates endocrine imbalances affecting body composition, mood regulation, and energy homeostasis.
Physical activity provides measurable benefits for hormone regulation. However, exercise prescription requires individualized approaches. Sedentary lifestyles contribute to the development of insulin resistance, while excessive high-intensity training may elevate stress hormone production. Dr. Stile recommends structured resistance training combined with moderate cardiovascular activity and parasympathetic nervous system activation practices for optimal endocrine support.
Lifestyle interventions alone may prove insufficient for specific hormone imbalances. Advanced hormone replacement protocols may become clinically indicated. DrStileRx.com offers specialized hormone testing panels to identify specific endocrine disruptions, enabling the development of individualized treatment strategies. These protocols may include bioidentical hormone replacement that matches endogenous hormone molecular structures for enhanced safety and efficacy profiles.
Hormone health presents unique individual variations. Chronological age, biological sex, lifestyle factors, and medical history create distinct endocrine profiles for each patient. Dr. Stile and the DrStileRx hormone optimization program recognize these variables and deliver precision medicine approaches rather than standardized treatment protocols.
Hormone optimization begins with clinical awareness and patient education. Early recognition of symptoms, combined with appropriate laboratory evaluation, enables intervention before significant impairment of quality of life occurs. Unexplained fatigue, body composition changes, mood dysregulation, or sleep architecture disruption may indicate endocrine dysfunction—the DrStileRx team provides specialized expertise to restore optimal hormone function and support long-term wellness goals.
Key Takeaways
Understanding and achieving hormonal balance is essential for optimal health, as hormones control virtually every bodily function from metabolism to mood.
• Recognize the warning signs early: Persistent fatigue, unexplained weight changes, mood swings, and sleep disturbances often signal hormone imbalances requiring professional evaluation.
• Prioritize lifestyle fundamentals: Quality sleep, stress management, regular exercise, and a nutrient-dense diet form the foundation of natural hormone optimization.
• Focus on hormone-supporting nutrition: Emphasize fiber-rich foods, healthy fats, complete proteins, and limit processed foods to support your body’s hormone production naturally.
• Consider professional testing when symptoms persist: Comprehensive hormone testing identifies specific imbalances, enabling personalized treatment plans including bioidentical hormone therapy when lifestyle changes aren’t sufficient.
• Balance is key in exercise: Combine strength training with moderate cardio and mind-body practices, avoiding excessive high-intensity workouts that can elevate stress hormones.
The path to hormonal wellness requires a personalized approach that addresses your unique hormone profile, lifestyle factors, and health goals through evidence-based strategies and professional guidance when needed.
Take the Next Step:
Please fill out the form on this page to request an in-person consultation, and one of our knowledgeable medical staff members at DrStileRx will reach out to you promptly. You can also call our office directly at (702) 940-9925.
DrStileRx serves Las Vegas, NV & Surrounding Areas.
*Individual results may vary
FAQs
What are some practical ways to naturally balance hormones?
Eating a nutrient-dense diet rich in fiber, healthy fats, and complete proteins can support hormone production. Regular exercise, quality sleep, and stress management techniques like meditation are also crucial for maintaining hormonal balance. Additionally, limiting exposure to environmental toxins and endocrine disruptors can help optimize hormone function.
How does stress impact hormone levels?
Chronic stress can significantly disrupt hormonal balance by constantly activating the body’s stress response system. This leads to elevated cortisol levels, which can interfere with other hormones, such as thyroid, estrogen, and testosterone. Managing stress through relaxation techniques, exercise, and proper sleep is essential for maintaining healthy hormone levels.
When should someone consider hormone replacement therapy?
Hormone replacement therapy (HRT) may be considered when persistent symptoms of hormone imbalance significantly affect quality of life, and lifestyle changes haven’t provided sufficient relief. It’s typically most beneficial when started before age 60 or within 10 years of menopause. However, the decision should be made in consultation with a healthcare provider after thorough evaluation and testing.
How can diet affect hormone balance?
Diet plays a crucial role in hormone regulation. Consuming a balanced diet rich in whole foods, lean proteins, healthy fats, and fiber can support optimal hormone production and function. Certain foods, such as soy, flaxseeds, and cruciferous vegetables, contain compounds that may influence hormone levels. Conversely, excessive sugar, processed foods, and alcohol can disrupt hormonal balance.
What role does exercise play in hormone regulation?
Regular exercise significantly impacts hormone balance. It can help regulate insulin levels, boost growth hormone and testosterone production, and reduce stress hormones like cortisol. Different types of exercise affect hormones differently—strength training can increase growth hormone and testosterone. At the same time, moderate cardio and mind-body practices like yoga can help lower cortisol levels and improve overall hormonal balance.
What are the signs of hormonal imbalance?
Signs of hormonal imbalance can include irregular periods, mood swings, fatigue, weight gain, and difficulty sleeping. Women may also experience symptoms related to reproductive health, such as hot flashes or changes in libido. Recognizing these symptoms early is crucial for managing hormonal health effectively.
How can I help balance hormones naturally?
To help balance hormones naturally, consider incorporating healthy fats into your diet, reducing processed foods and excess sugar, and managing stress levels. Engaging in regular physical activity and ensuring adequate sleep can also support hormonal health. Additionally, certain herbs and supplements may help regulate your hormones.
What health conditions are associated with hormone imbalance?
Several health conditions are directly associated with hormonal imbalances, including polycystic ovary syndrome (PCOS), thyroid disorders, and adrenal fatigue. These conditions can lead to various symptoms that affect overall health and well-being, making it essential to seek diagnosis and treatment from a healthcare professional.
How do hormones play a crucial role in overall health?
Hormones are chemical messengers that regulate numerous bodily functions, including metabolism, mood, and reproductive health. Keeping your hormones in check is vital for maintaining a balanced diet, managing weight, and ensuring optimal mental health. Hormones may influence everything from energy levels to immune function.
What are some expert tips to improve your hormonal health?
Expert tips for improving hormonal health include maintaining a balanced diet rich in whole foods, managing stress through mindfulness practices, and ensuring regular physical activity. Incorporating foods that support thyroid hormone levels, such as iodine-rich foods, can also be beneficial. Regular check-ups and hormone level tests are recommended.
What are the symptoms of a hormonal imbalance in women?
Symptoms of a hormonal imbalance in women can manifest as irregular periods, mood changes, weight fluctuations, and fatigue. Other signs may include acne, hair loss, and changes in libido. It’s essential to consult a healthcare provider if you experience these symptoms to ensure proper diagnosis and treatment.
How can diet help balance hormones?
A balanced diet rich in nutrients can significantly help balance hormones. Including healthy fats, fiber, and proteins while minimizing processed foods and excess sugar can regulate hormones effectively. Foods high in omega-3 fatty acids, antioxidants, and fiber can also support hormonal health and improve overall well-being.
What tests are available to check hormone levels?
There are several tests available to check hormone levels, including blood tests that measure levels of estrogen, progesterone, testosterone, and thyroid hormones. Saliva and urine tests can also provide insights into hormone balance. Consulting with a healthcare provider can help determine which tests are appropriate based on your symptoms and health conditions.

